Researchers at the UCSD School of Medicine have finally found a viable way to utilize the staurosporine compound as an anti-cancer drug after years of roadblocks by various unwanted side effects and unknown effective delivery paths.
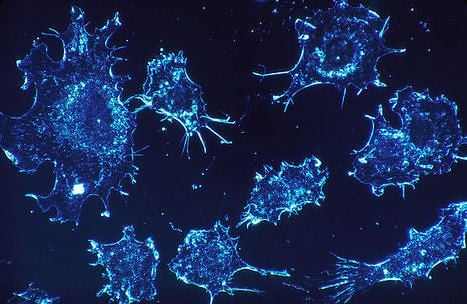
The compound — taken from the Streptomyces staurosporeus bacterium — works by inducing self-destruction in cancer cells.
“Basically, people have been working with the compound for three to four decades to make it into a viable drug, but it’s been limited because it’s very toxic and highly protein-bound,” UCSD Moores Cancer Center Director of Neuro-Oncology Santosh Kesari said.
Kesari said that if too much STS is given, the cells affected will consequently undergo cell death, and if too little STS is given, the compound will naturally bind to lingering proteins and have no efficacy.
Scientists in the past were aware of the potential that STS had and tried to alter the compound to make it available for cancer patients. Modification results tended to be less toxic towards cancer cells and were clinically ineffective to humans. Researchers also attempted to use liposomes, but the delivery system was not refined.
Complications led to the National Cancer Institute to abandon the research, but upon revisiting the NCI Clinical Collection, UCSD researcher Dr. Rajesh Mukthavaram noted that STS was one of the top compounds to kill glioblastoma (highly malignant cancer found in the brain). This fact inspired Kesari and his associates to overcome the past obstacles of deliverance.
After spending two years on the three-year project, Kesari solved the issue by perfecting the previously attempted liposomal technology.
“It’s a hot button thing — repurposing compounds we already know,” Kesari said. “Take a lot of these drugs similar to STS and put it into a liposome to overcome the pharmacokinetic barriers.”
Liposomes, artificially created and lipid-bound vesicles, are packaged with STS and then released in the body. The liposomes selectively travel to the tumor and dump the toxic payload, all without affecting normal cells. Being able to properly administer STS maximizes its potential, which is STS’s ability to deal with solid and liquid tumors. Soon-to-be-published research also shows that STS can reach brain tumors directly, a normally difficult area for cancer treatment.
“We were thrilled to be able to retool this compound that’s been around for decades in a novel way to be used for the future,” Kesari said about his findings.
The team’s research has a patent on it and a company ready to license the drug. Within the next two years, Kesari is hoping to see STS used as a new anti-cancer drug for clinical trials and patients alike.








Complete Health Care in Florida • Nov 13, 2013 at 9:14 am
A very informative article to read… thanks for the article and the awareness